GAP President John Dwyer was featured in Pink Sheet talking about the cost of Aduhelm affecting the Centers for Medicare and Medicaid Services NCD.
US Medicare coverage policy is supposed to be fenced off from considerations about the cost of a prescription drug (or other item or service). But the notion that the cost of Biogen, Inc. and Eisai Co., Ltd.’s Aduhelm was a factor in Medicare’s proposed national coverage policy for Alzheimer’s drugs continues to surface in the debate over the policy.
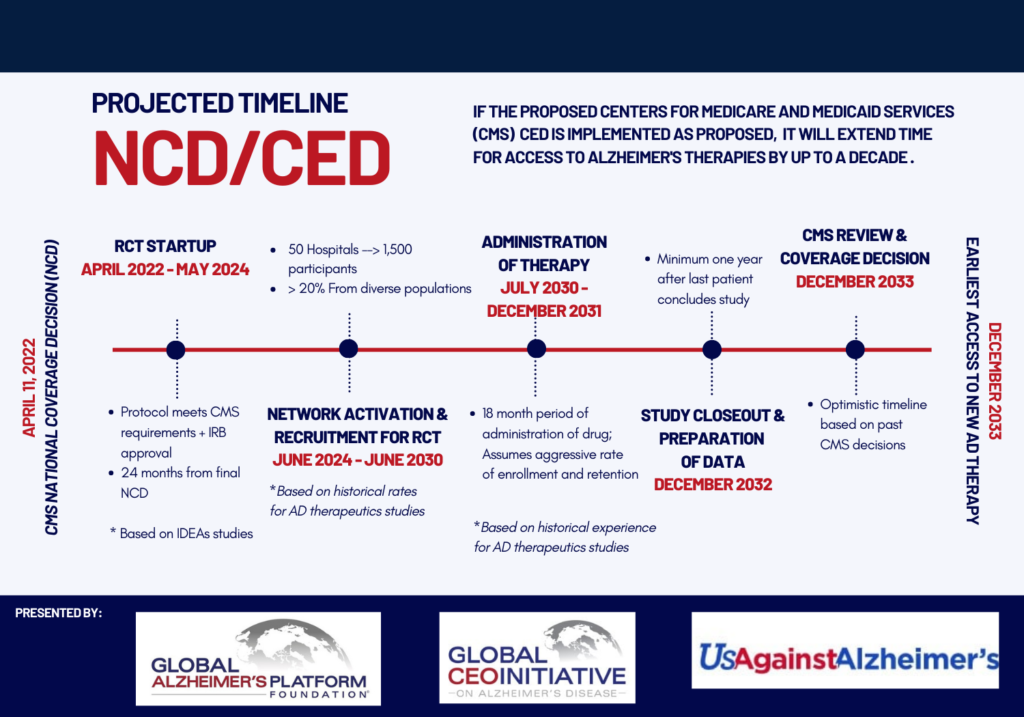
The Centers for Medicare and Medicaid Services released a draft national coverage determination 11 January proposing that Medicare coverage for amyloid-directed monoclonal antibody drugs including Aduhelm would be restricted to use in randomized clinical trials, an approach known as coverage with evidence development. (Also see “Medicare Draft NCD For Alzheimer’s Drugs: When ‘Reasonable And Necessary’ And ‘Safe And Effective’ No Longer Align” – Pink Sheet, 11 Jan, 2022.)
Critics of the decision have been vocal about their concerns that the policy represents an attempt to ration access to the drugs based on cost concerns and could be a sign of things to come. Aduhelm now costs an average of $28,000 per year following Biogen’s recent decision to reduce its price by nearly half. (Also see “Who Needs The BBB? Aduhelm Shows Medicare Price ‘Negotiation’ Is Already Here” – Pink Sheet, 21 Dec, 2021.)
In a recent editorial in the Wall Street Journal, former US Food and Drug Administration commissioner (and CMS senior advisor) Scott Gottlieb wrote that Aduhelm “has become an example for critics who bemoan the rising cost of medicines to treat serious conditions and the limited data that often accompany innovative products when they first win FDA approval.”
He pointed out “many drug industry critics applaud Medicare’s muscular response,” but cautions “the risk is that public health agencies will routinely make such political decisions. Regulators are increasingly focused on the price of drugs even though such considerations fall outside Medicare’s legal mandate.”
Alzheimer’s patient advocate and clinical trials expert John Dwyer also argued that cost played a key role in the CMS decision during a recent webinar hosted by the Alliance for Aging Research. (Also see “Medicare May Scale Back Coverage Restrictions For Alzheimer’s Drugs; Will It Be Enough?” – Pink Sheet, 11 Feb, 2022.)Dwyer is president of the Global Alzheimer’s Platform Foundation.
Despite CMS statements that its draft policy responds to a lack of evidence on clinical effectiveness and safety concerns, “this isn’t about safety,” he said. “It’s about the size of the patient population. There are just too many Alzheimer’s patients. When you look at trying to pay for hundreds of thousands or one million people that could benefit from this drug, it causes the agency a great deal of angst and I think that is clearly in play.”
Even supporters of the draft decision are making a connection between the proposed policy and cost. The Medicare Payment Advisory Commission raised the issue in 10 February comments to the agency.
The fact that MedPAC submitted comments to CMS on a Medicare coverage policy is unusual, as the group notes. But “we have chosen to do so in this case because of its significance, including the potential fiscal implications, and because the decision invokes coverage with evidence development, which we have discussed in the context of our prescription drug work,” the comments explain.
“Although Medicare payment implications are outside the scope of an NCD, Aduhelm has highlighted the broader challenges Medicare faces in paying for high-cost products with limited clinical evidence,” MedPAC says.
“At the current price of $28,200 for a year of maintenance therapy, Medicare Part B [fee-for-service] spending and beneficiary cost sharing could total $1.5bn annually if 50,000 FFS beneficiaries received the product and $1.5bn annually if 500,000 FFS beneficiaries received the product. Thus, with substantial uptake, the product has potential to swamp current Part B drug spending, which totaled $39bn in 2019.”
In addition to spending on Aduhelm alone, treatment “is likely to increase use of, and therefore spending on, MRIs … and potential PET scans,” which are used to guide administration and monitor for safety, the advisory group points out.
MedPAC has had its eye on Aduhelm for some time. The group discussed approaches including coverage with evidence development for containing the cost of the drug and other physician-administered treatments covered under Part B during an October 2010 meeting. (Also see “MedPAC’s Part B Options Include ‘Value-Based’ Payment During Accelerated Approval” – Pink Sheet, 18 Oct, 2021.)
A group of drug policy experts known as the Council for Informed Drug Spending Analysis also applauded the CMS draft decision as a way to help control drug costs in separate comments to the agency.
The council is chaired by Sean Dickson, director of health policy at West Health Policy Center, and includes academics without ties to the pharmaceutical industry such as Rachel Sachs (Wash. U. law school) and Stacie Dusetzina (Vanderbilt), who is also a MedPAC commissioner. Also part of the group is Richard Frank, former assistant secretary for planning and evaluation at the Health and Human Services Department. Frank is now director of the USC-Brookings Schaeffer Initiative on Health Policy.
“While we recognize that neither the cost of anti-amyloid mAbs themselves nor their overall spending implications for the Medicare program are a component of CMS’ ‘reasonable and necessary determination,’ we believe that an appropriate use of the reasonable and necessary criteria will have an important effect on Medicare spending, patient out-of-pocket costs, and the pricing trends for new anti-amyloid mAbs,” the group says.
Therefore, “the rigorous standards proposed are an essential component in not only developing the future evidence necessary to determine whether anti-amyloid mAbs are indeed clinically efficacious, but also to manage drug spending and address ever-rising launch prices of clinician-administered therapies.”
Former CMS administrator ad FDA commissioner Mark McClellan discussed whether cost concerns were behind the CMS draft decision during the BIO CEO & Investor conference 15 February. “CMS went out of their way in the review to say not only are we not allowed to look at [cost], we’re not looking at it” and “I don’t think cost was in this directly,” McClellan pointed out. He is now director of the Duke-Margolis Center for Health Policy.
“That said, obviously cost implications are going to be bigger for populations that are much broader and populations that are much broader are going to tend to raise more issues about [whether] this treatment really works well in all of these patients,” he observed. “MedPAC and many other groups [in their comments] were very explicit in saying this is a lot of money to spend on treatments where the evidence is more limited than we’d like it to be.”
Originally posted by Pink Sheet on February 16, 2022.